Parkinson’s, Alzheimer’s, depression… is a stool transplant the solution?
The science suggests it might be
Unless you’ve spent the last few years in a coma, you’ll know that awareness of the role of the gut microbiome in maintaining overall health has gone mainstream. The microbiome is (almost) front page news and on every media platform.
It’s also on shop shelves: from probiotic supplements to prebiotic food and drinks, gut bacteria have finally achieved the recognition and acclaim they deserve.
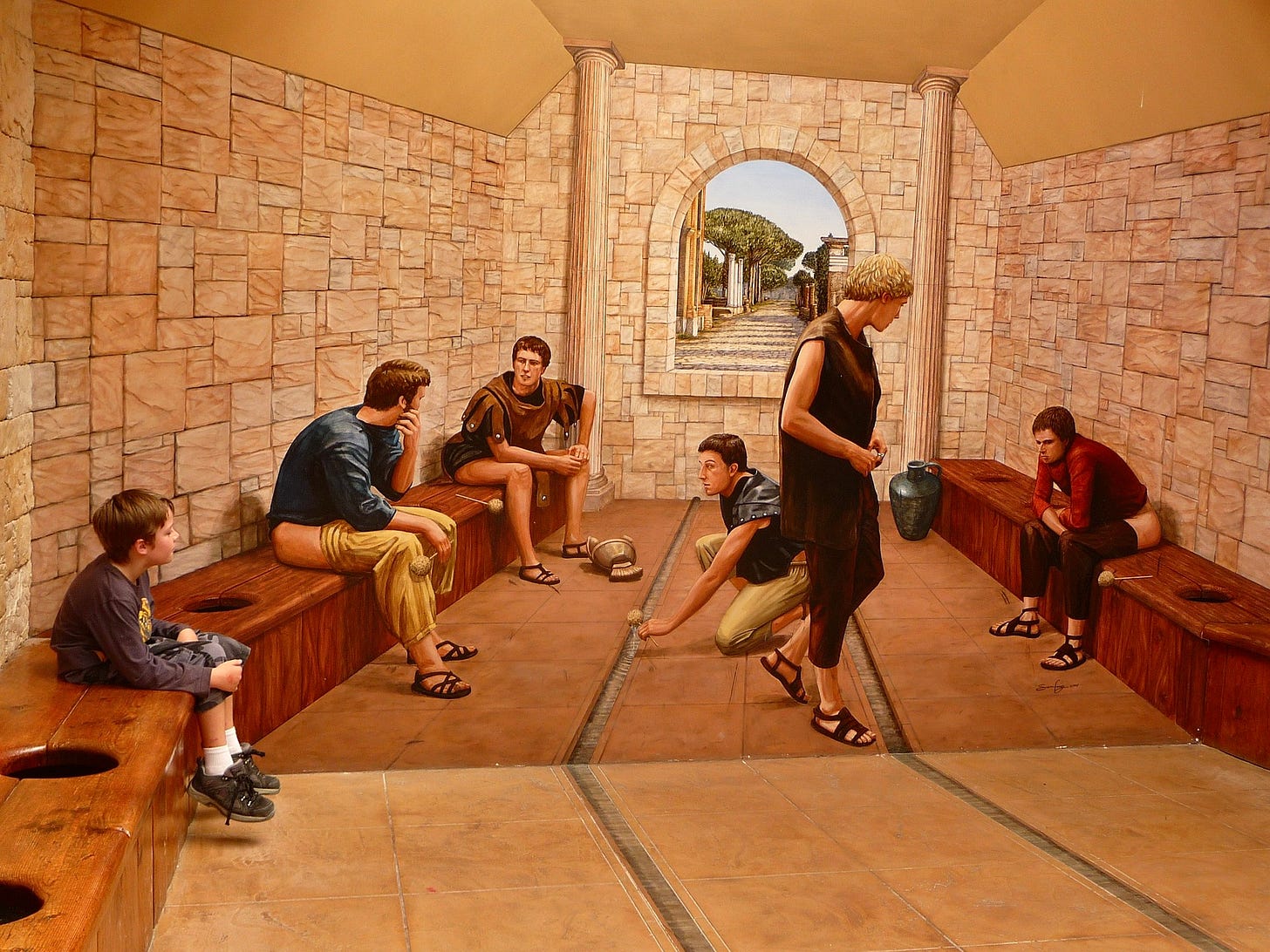
So what’s next? Where do we go from here? To stool transplants, that’s where. Just like blood or organ transplants, faecal microbiota transplant (FMT) is already happening. It means that you can bypass the usual routes to increasing friendly bacteria and simply have an implant of someone else’s faecal matter, someone whose gut is in better condition than your own.
Before you faint from the yuck factor, be aware that this is not a passing trend or weird niche interest: FMT is a US Food and Drug Administration-approved medical procedure that can save lives.
It works like this: faecal matter is collected from a healthy donor (usually a spouse or close relative) and implanted into the recipient, thus altering the composition of bacteria and other living organisms in the gut.
FMT was approved by the FDA in 2013 as a treatment for recurrent and refractory Clostridium difficile bacterial infection. C. diff frequently arises after a course of antibiotics and is often fatal, especially among the elderly. The success rate of FMT in treating C. diff is well over 90%; the success rate of antibiotic therapy is only 20-30%.
No wonder researchers are keen to explore other areas of health that may benefit from this safe and cost-effective treatment. And with what we already know about the gut-brain connection, and the role that gut bacteria play in influencing the mind, FMT has sparked a special interest in the field of mental and neurological health research.
“Many successful cases of FMT in the treatment of neurological diseases/psychiatric diseases often have obvious GI (gastrointestinal) symptoms, and the improvement of neurological symptoms/mental symptoms is also related to the GI symptoms.”
From depression to Alzheimer’s and Parkinson’s, the emerging research is looking more than a little promising.
Keep reading with a 7-day free trial
Subscribe to Your Nutritionist Recommends to keep reading this post and get 7 days of free access to the full post archives.